| <<< Previous | Index | Next >>> |
Case 5 and 6 (To be discussed together)
Case 5
Clinical and haematological data.
54-yr-old woman. Rheumatoid arthritis (RA) since 12 yrs, treated by chloroquin.
Presented with splenomegaly, anaemia, neutropenia and thrombocytopenia.
No peripheral adenopathy, but mediastinal and retroperitoneal adenopathy at CT-scan. Hepatomegaly. Lymphoma suspected.
BM aspirate : lymphocytic infiltrates on 8 / 10 smears, without significant atypia
.
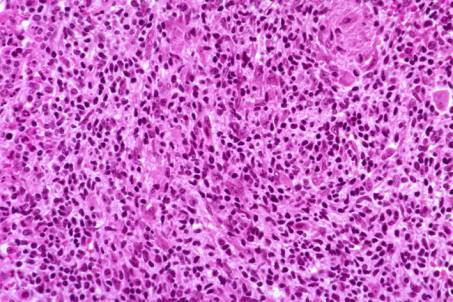
BM biopsy: Overall increased cellularity. Granulocytic cell line predominant. Lymphoid foci
- intertrabecular and occasionally paratrabecular- with atypical small to medium-sized lymphocytes with irregular nuclear contours and condensed chromatin. Granulomatous reaction associated with the lymphoid foci. Increased number of eosinophils. No microorganisms detected by special stains. Increase of the reticulin.
On IHC preparation, positivity of the atypical lymphoid cells for CD3. Rare CD20 positive B-cells. No CD30 positive cells. Numerous histiocytes coloured by CD 68/PGM1.
Molecular biology: no monoclonal rearrangement could be found by PCR.
Interpretation and diagnosis: picture raising a differential diagnosis between a T-cell lymphoma, a T-cell rich B-cell lymphoma and Hodgkin's disease. Reactive process less probable because of the cell atypia.
Because of the IHC results, BM histology most consistent with a peripheral T-cell lymphoma. Non specific granulomatous reaction.
PB smears reviewed later on: Moderate lymphocytosis. Presence of Large Granular Lymphocyte (LGL) with azurophilic granules. Flow cytometry: 95 % CD3+ lymphocytes, with 83 % lymphocytes presenting a coexpression CD3/ CD57
Final diagnosis : LGL leukaemia.
Case 5. Large Granular Lymphocyte Leukaemia.
Clinical and haematological data.
53-yr-old woman. Presented with pulmonary abscess and pseudomonas aeruginosa septicaemia. Splenomegaly. No adenopathy. Neutropenia.
Hb 88 g/l, L 7 G/ l, T 209 G/l
Neutrophils 4.6 %, Lymphocytes 86.9 %, Monocytes 7.6 %
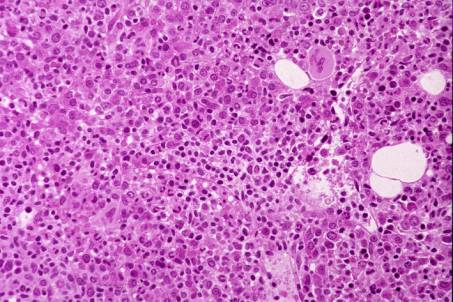
BM biopsy was performed because of suspicion of lymphoma or of Myelodysplastic Syndrome. BM trephine shows an overall increased cellularity. Erythrocyte cell line present with minor dysplastic changes. Shift to the left of the granulocytic cell line. Moderate increase of the number of megakaryocytes without any significant atypia. On HE section, a few clusters of lymphocytes are to be seen. Some lymphocytes exhibit an irregular or indented nucleus. Few plasma cells. Moderate increase of the reticulin network.
Lymphocytosis much more apparent on IHC preparations. Clear-cut predominance of CD3 and CD8 T-cells.
Molecular biology : a monoclonal TRC-
g
rearrangement was demonstrated by PCR.
Interpretation and diagnosis : on HE section, the picture could be suggestive of a reactive process - due to infection and/or hypersplenism - with hyperplastic BM and lymphoplasmacytosis. However, because of the IHC and molecular results, a diagnosis of peripheral T-cell lymphoma is favoured.
PB smears reviewed (2 nd look) : about 50 % lymphocytes of the Large Granular Lymphocyte (LGL) type (azurophilic granules).
At flow cytometry, 98 % lymphocytes CD3+, with 88% of them co-expressing CD8 and 57 % CD57.
Final diagnosis : LGL leukaemia
Case 6. Large Granular Lymphocyte Leukaemia.
Comments
LGL leukaemia does not have distinctive features on BM biopsy and can be confused with a reactive process or various small cell lymphoproliferative disorders. The BM lymphocytic infiltration may be subtle and difficult to detect if IHC is not applied. Simultaneous examination of the PB smears and complementary investigations such as flow cytometry are necessary to recognize the disease.
Clonal diseases of LGL disorders can arise from a CD3+ T-cell lineage or from a CD3 - NK-cell lineage. According to Lamy and Loughran (1999), CD3+ LGL leukaemia is the most frequent form of LGL leukaemia. It is a disease of elderly people. Approximately 60 % of patients are symptomatic: recurrent infections secondary to chronic neutropenia, anaemia, and RA. In the recent paper by Lamy and Loughran it is suggested that "dysregulated apoptosis could be an underlying mechanism for both malignancy and autoimmune disease".
| <<< Previous | Index | Next >>> |
Copyright 2001, The Author(s) and/or The Publisher(s)
| Organisation: FORPATH asbl |
Coordination: Dr Bernard Van den Heule |
Host: Labo CMP |