| <<< Previous | Index | Next >>> |
Case 2
Clinical and haematological data.
53 yr-old women. Presented with polyadenopathy and hepatosplenomegaly.
Hb 109 g/l, L 4.9 G/l, T 117 G/l
A few "atypical" lymphocytes observed on the PB smear.
BM aspirate : overall BM cellularity normal; lymphocytic infiltration (40%); lymphoma suspected.
A bilateral BM biopsy is performed.
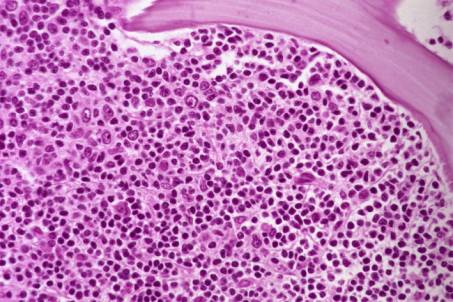
Both biopsies are characterized by focal and paratrabecular large lymphoid infiltrates; some of them coalescing and becoming diffuse, exhibiting predominantly small to medium sized lymphocytes - many of them with "cleaved" nuclei" - associated with a few blasts (isolated cells or small clusters). Interstitial spillage of the lymphoid cells in the residual surrounding haemopoietic tissue. Reticulin fibres significantly increased..
IHC: Lymphoid infiltration positive for B-cell markers (CD20/L26 and DBB42); minority of CD3 +T-cells.
Interpretation and diagnosis.
Focal and diffuse infiltration of the BM biopsy by a predominantly small B - cell lymphoma with paratrabecular involvement consistent with a Follicular Lymphoma (FL) (REAL/WHO).
Comments
Pattern and morphology typical of FL.
The differential diagnosis usually encompasses other types of small B-cell lymphomas, mainly mantle cell lymphoma. The lymphoid population in MCL is usually more uniform. In this particular case, a cervical LN biopsy revealed a FL grade 3.
Patients with Follicular Centre Cell lymphoma (FCCL) usually present with advanced disease
. BM involvement is frequently detected, even when the PB is normal. BM involvement is more common in the predominantly small cell variant : 50-85 % of the cases, according to different series. Leukaemic cells may be recognized in PB smears in a minority of cases. Lymphocytosis > 5 G/l, which could be confused with B-CLL is recognized as part of FCCL by the presence of notched nuclear cells. BM aspirate is often not representative due to patchy infiltration and increase in reticulin fibres in the neoplastic areas.
On histological sections, BM involvement is usually patchy with a characteristic
paratrabecular pattern . A focal nodular ("non-paratrabecular") pattern may be observed in some cases and raises a difficult differential diagnosis with reactive or benign lymphoid nodules (see
Table 4). The
reticulin is significantly increased in direct relationship to the degree of cellular infiltrate. The infiltrates are composed of
small - to medium size cells with numerous "cleaved" forms and a minority of blast cells, which are strongly stained by B-cell markers. When histology is inconclusive, the precise immunophenotype has to be defined by flow cytometry.
Remember that the follicular architecture of the lymphoma is not identified on BM sections. A LN biopsy is recommended. Cellular composition may vary from one site to another and discrepancy between BM and lymph nodes may be observed. The more aggressive pattern is usually seen on the lymph node.
Case 2. Follicular Lymphoma.
| <<< Previous | Index | Next >>> |
Copyright 2001, The Author(s) and/or The Publisher(s)
| Organisation: FORPATH asbl |
Coordination: Dr Bernard Van den Heule |
Host: Labo CMP |