| <<< Previous | Index | Next >>> |
Case 3
Clinical and haematological data.
57-yr-old man. No hepatosplenomegaly and no adenopathy.
Hb 137 g/l, L 19 G/l, T 208 G/l.
80 % lymphocytes without significant atypia on PB smear.
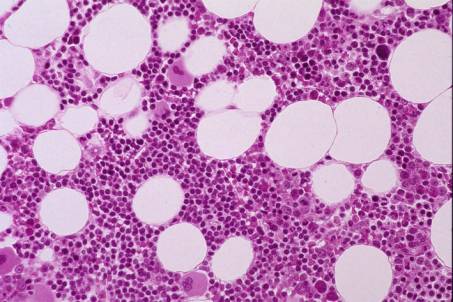
At low power, the BM biopsy shows a global cellularity within normal range, although somewhat heterogeneous. Three cell lines present with maturation. Closer inspection reveals an interstitial infiltration by small lymphocytes with occasional nodular condensation and no significant atypia. In some areas, the haemopoietic cells are interspersed with lymphocytes.
IHC . The majority of lymphoid cells are positive for B-cell markers, DBB42 and CD45RA; only weak positivity for CD20. A minority of lymphocytes are CD3+ T - cells.
Interpretation and diagnosis .
B-cell infiltration of BM, predominantly interstitial, consistent with Chronic Lymphocytic Leukaemia
(CLL)
Comments
This case illustrates the interstitial or early pattern of BM infiltration by CLL. Careful morphological and IHC examination are required for a correct interpretation.
Diagnosis of B-CLL is based on laboratory studies which include a full blood count with careful attention to the morphology of the lymphocytes, a BM aspirate and trephine biopsy and a minimum of cell markers (flow cytometry and/or BM biopsy). Persistent lymphocytosis over 10 G/l without apparent cause seems necessary for the diagnosis. Blood film exhibits a predominance of small lymphocytes with scanty cytoplasm, round nucleus, clumped nuclear chromatin and absence of azurophil granules.
Four histological patterns of BM infiltration have been described 1) interstitial, 2) focal / nodular, 3) mixed interstitial and focal / nodular and 4) diffuse.
The diffuse pattern represents the most advanced degree of infiltration with complete replacement of BM spaces. The pattern - diffuse versus non diffuse - has been shown by some authors to represent a significant prognostic parameter.
Small lymphocytes are usually predominant in the BM infiltrates. A minority of prolymphocytes (PL) and/or immunoblast-like cells are usually observed. Clusters of prolymphocytes or so called "proliferative centres" resembling those observed on lymph node biopsy- may be seen in some cases. There is little if any increase in reticulin. Two types of
transformation have been recognized in B-CLL and can occasionally be detected on BM biopsy: prolymphocytoid and large B-cell lymphoma (so-called "Richter's Syndrome").
The differential diagnosis includes:
- Reactive lymphocytosis . Usually characterized by a mixture of B- and T-cells, but reactive B-lymphocytosis may occur (mainly in autoimmune diseases or viral infection). Flow cytometry may be necessary to assess clonality.
- Other B-cell lymphoproliferative disorders, small cell type, such as Hairy Cell Disease
(positivity for DBA.44), Immunocytoma (monotypic plasma cells), Mantle Cell Lymphoma (should be positive for PRAD1/Cyclin D1), Splenic Marginal Zone Lymphoma. In difficult situations, flow cytometry required (Table 3).
- to confirm the diagnosis and exclude other lymphoproliferative diseases
- to define the pattern of BM infiltration
- to assess the BM haemopoietic capacity in relation to the peripheral blood findings
- to detect morphological changes of B-CLL.
Case 3. Chronic Lymphocytic Leukaemia (CLL).
| <<< Previous | Index | Next >>> |
Copyright 2001, The Author(s) and/or The Publisher(s)
| Organisation: FORPATH asbl |
Coordination: Dr Bernard Van den Heule |
Host: Labo CMP |